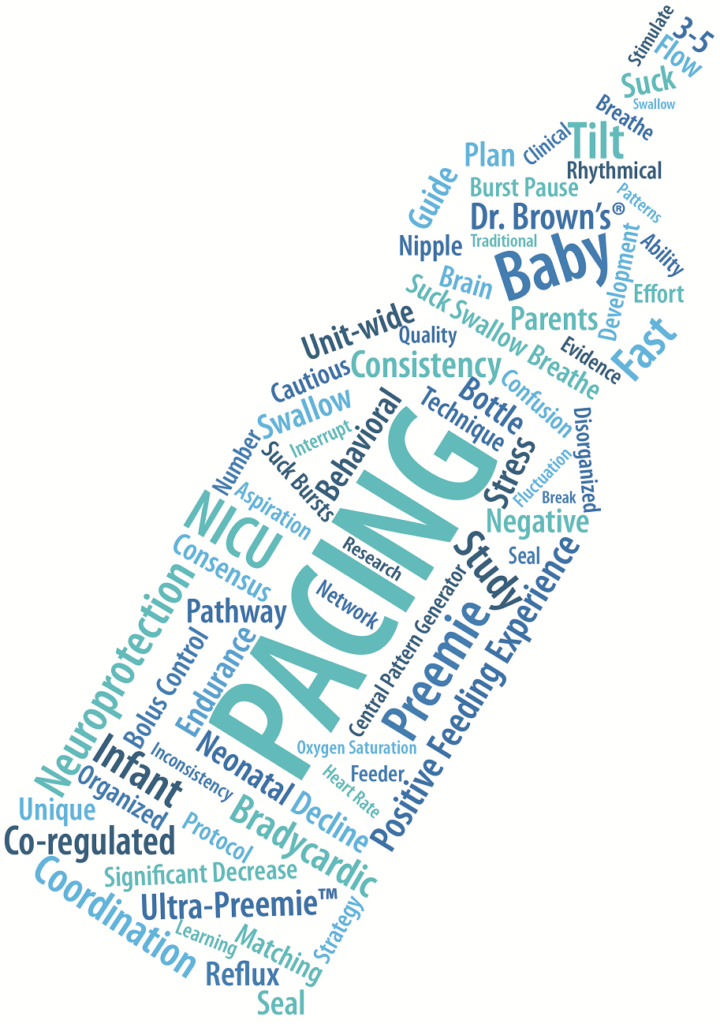
Over the years, NICU professionals have used Pacing as a strategy to assist infants who are learning the complex task of coordinating sucking, swallowing, and breathing. Initially, Rosen, Glaze, and Frost (1984) first noted in their study of hypoxemia during feeding of vulnerable infants that interrupting the infant’s sucking when breathing was irregular resulted in a return of regular breathing and increased oxygen levels. Palmer (1993) developed a protocol of paced feeding which guides the feeder to regulate the number of sucks per burst and the duration of bursts and pauses by removing the nipple from the infant’s mouth every 3-5 sucks to impose breathing pauses.
Over the years, NICU professionals have used Pacing as a strategy to assist infants who are learning the complex task of coordinating sucking, swallowing, and breathing. Initially, Rosen, Glaze, and Frost (1984) first noted in their study of hypoxemia during feeding of vulnerable infants that interrupting the infant’s sucking when breathing was irregular resulted in a return of regular breathing and increased oxygen levels. Palmer (1993) developed a protocol of paced feeding which guides the feeder to regulate the number of sucks per burst and the duration of bursts and pauses by removing the nipple from the infant’s mouth every 3-5 sucks to impose breathing pauses.
A study by Law-Morstatt et al (2003) using this protocol involved a nonrandomized clinical trial of 36 infants, comparing ‘traditional’ bottle-feeding with the paced feeding protocol. The paced infants demonstrated statistically and clinically significant decreases in bradycardic incidences during feeding and gains in development of more efficient sucking patterns at discharge.
This concept developed further with Shaker (2017) and Thoyre (2012) as ‘coregulated pacing.’ This type of pacing is individualized throughout the feeding, dependent on the infant’s ability to breathe with sufficient rate and depth and to swallow safely. The goal of the feeder is not only to respond to the infant’s need for additional breathing or reorganization, but also to learn about the infant’s patterns and signals, or cues, so that the feeding rhythms can be co-regulated proactively. In a study by Thoyre et al (2012), results indicated that infants fed with a coregulated approach had less SaO2 variability, decline, and time spent in a desaturated state; less heart rate fluctuation and decline; less behavioral disorganization; better fluid management; and less observed effort to breathe.
While pacing is used as a supportive strategy by many neonatal care providers, there can be some disadvantages, and some experts have suggested to use cautiously. Because the method of pacing varies, it can be difficult to be consistent among caregivers. For example, there are several ways to pace an infant, including tilting the bottle, tilting the baby, breaking the seal, or removing the bottle. Each of these methods has their advantages and disadvantages (Ferrara 2018). It is essential that if pacing is used in a NICU, that there is a unit-wide consensus on which technique is used. The CoReg Feeding Approach Protocol, (2012) for example, outlines ways to incorporate consensus and includes specific instructions for how and when to provide pacing.
There are other disadvantages of pacing, depending on how it is completed:
- Pacing can be a source of stress and confusion for parents; it can be poorly timed since the bottle is removed after stress has already occurred, and can disrupt the suck/swallow/breathe pattern if removing the bottle (Fuller 2017)
- Further, if we are disrupting the normal process of an infant learning about this pattern, are we altering brain pathway formation and network tuning related to the Central Pattern Generator?
- If you are only tilting the bottle, this can stimulate the suck reflex. If the infant continues to suck it may increase reflux (Ferrara 2018)
- Breaking the seal only can create abnormal sensory input to gums/buccal pads (Ferrara 2018)
Due to some of the inconsistencies and disadvantages with pacing, Fuller (2017) has suggested that matching the flow rate to the infant’s ability could eliminate/reduce the need for external pacing. In her practice, she has found that the use of the Ultra-Preemie™ nipple on the Dr. Brown’s bottle system allows the flow rate to be slow enough that infants can begin to regulate their breathing on their own and not require external pacing.
Pacing has historically been used as one method of improving coordination of suck/swallow/breathe for infants but should be used cautiously and with more intentional planning. Of course, every infant is unique, and our therapeutic strategies should reflect this. If you incorporate pacing in your practice, aim for consistency and education for all caregivers feeding the infant.
Click here for references.
*In the second part of this series, the results of a survey provided to NICU professionals on current pacing strategies and practice will be revealed. If you would like to participate, please go to: https://www.surveymonkey.com/r/VGC6LZD
This message is being shared by NANT on behalf of an external organization. Sharing this message is not indicative of endorsement or recommendation by NANT. The information presented in this message is not meant to serve as a guideline for patient management. Any products, procedures, or treatments discussed or suggested should not be used by clinicians without evaluation or their patients’ conditions and possible contraindications, review of any applicable manufacturer’s product information, comparison with recommendations of other authorities, and policies, procedures, and guidelines of clinicians’ place of employment.